As medical advancements continue to shape the field of cardiology, researchers have turned their attention to finding more effective and cost-efficient interventions for patients with acute myocardial infarction (MI) and multivessel disease. In a recent prespecified analysis of the FRAME-AMI trial, fractional flow reserve (FFR) guidance emerged as a potential solution that not only increases quality-adjusted life-years (QALYs) but also reduces healthcare costs. Led by Dr. Joo Myung Lee and his team at Samsung Medical Center in Seoul, South Korea, the study compared FFR-guided percutaneous coronary intervention (PCI) with angiography-guided PCI of non-culprit lesions. The findings, published in JAMA Network Open, shed light on how FFR guidance can significantly improve patient outcomes and economics in acute MI cases.
One of the most striking results of the analysis was the increase in QALYs associated with FFR guidance for complete revascularization. Compared to angiography-guided PCI, FFR guidance led to a gain of 0.06 QALYs per patient. This improvement in quality of life is undoubtedly a substantial benefit for individuals recovering from acute MI. Moreover, the study found that these gains were consistent across all key subgroups and applicable across different healthcare systems, including the U.S., Korean, and European systems.
In addition to its positive impact on patient outcomes, FFR guidance also demonstrated a cost advantage over angiography-guided PCI. The cumulative total cost per patient was $1,208 less when FFR was utilized. This reduction in cost can be particularly significant when considering the larger population of acute MI patients requiring intervention. With the incremental net monetary benefit of $3,378 and an incremental cost-effectiveness ratio of -$19,484, FFR guidance proves to be the more cost-effective strategy over a 4-year time horizon.
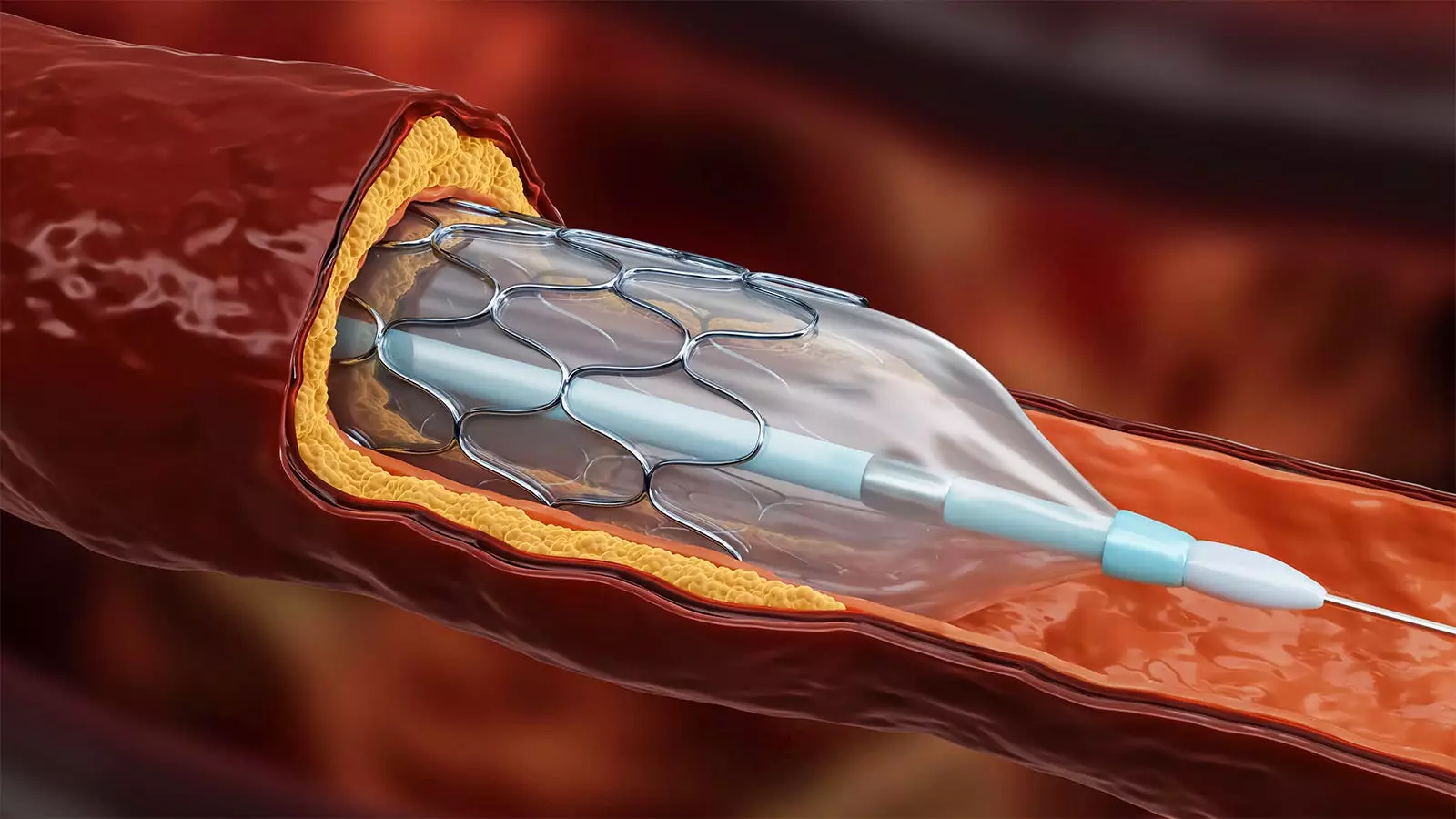
The study raises an important question regarding the routine use of angiography-guided PCI for non-infarct-related artery (IRA) lesions. According to Dr. Lee’s team, routine angiography-guided PCI, even for lesions with a diameter stenosis greater than 50%, may result in unnecessary procedures, additional stents, increased contrast media use, and higher risks of complications. These factors can potentially worsen long-term patient prognosis. On the other hand, FFR-guided PCI allows for more targeted interventions, avoiding unnecessary procedures for functionally insignificant stenosis. Therefore, FFR-guided PCI emerges as a superior approach for patients with stable ischemic heart disease and those with acute MI and multivessel disease.
The results of the FRAME-AMI trial strongly support the use of FFR guidance in determining which nonculprit lesions require intervention. In contrast to the FLOWER-MI trial, which did not find FFR superior to angiographic guidance, FRAME-AMI showed the overwhelmingly favorable results of FFR guidance. In the FFR-guided group, PCI was performed for non-IRA lesions in 64.1% of cases, while the angiography-guided group saw a significantly higher rate of 97.1%. Notably, deferring PCI for non-IRA based on FFR provided comparable or even superior clinical outcomes. The lower rates of non-IRA PCI with FFR-guided interventions underscore the potential for substantial savings in medical resources and costs without compromising patient safety or prognosis.
Implications for Future Clinical Practice and Policy
The cost-effectiveness data presented in the study are highly significant and can greatly impact clinical practice and policy decisions. Dr. Rushi Parikh and colleagues from the University of California Los Angeles emphasize the importance of these findings in informing the adoption of an FFR-based strategy to achieve complete revascularization and address rising costs in acute MI. However, they also acknowledge the need for larger trials powered for hard outcomes to further evaluate the preferred strategy in this evolving clinical paradigm. Nonetheless, the consistent cost-effectiveness of FFR-guided complete revascularization across different healthcare systems is a noteworthy advantage that may shape future policies.
While the FRAME-AMI trial and its subsequent cost-effectiveness analysis offer valuable insights, there are limitations to consider. The analysis relied on limited country-level healthcare system data, which may impact its generalizability. Additionally, the trial was halted prematurely due to the COVID-19 pandemic, limiting the number of patients included in the analysis. It is important to address these limitations in future research to ensure a comprehensive understanding of the economic benefits and clinical outcomes associated with FFR-guided PCI.
The findings of the prespecified analysis of the FRAME-AMI trial highlight the potential of FFR guidance in improving quality of life and reducing costs for patients with acute MI and multivessel disease. With its ability to increase QALYs and lower cumulative total costs per patient, FFR-guided PCI emerges as a promising strategy for achieving complete revascularization. Future research and larger trials will play a crucial role in determining the long-term clinical and economic benefits of FFR guidance. As the field of cardiology continues to evolve, strategies like FFR guidance hold great promise in optimizing patient care and resource utilization in acute MI cases.

Leave a Reply