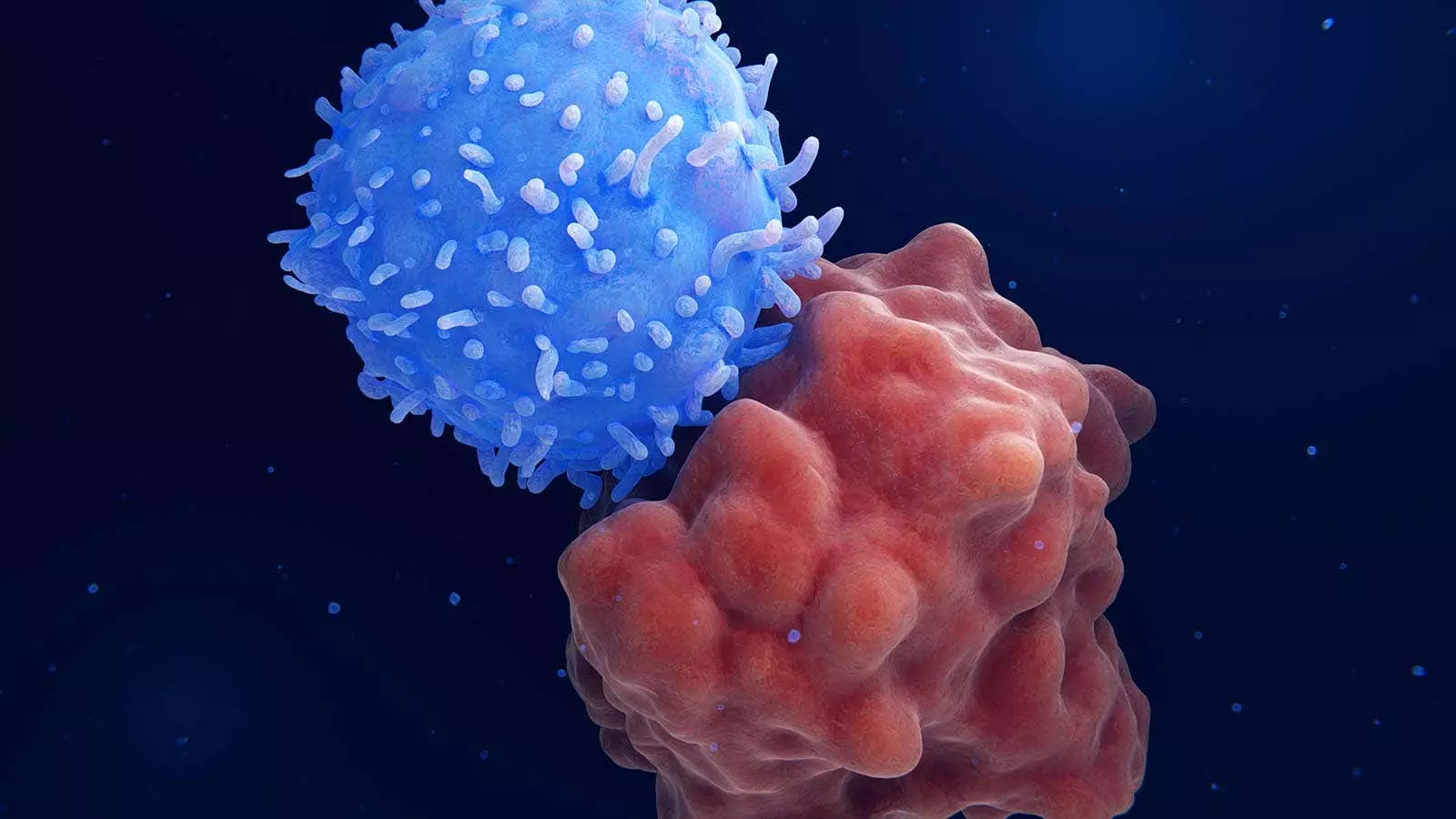
In a recent study conducted by Chinese researchers, a novel treatment strategy involving sequential CD7 chimeric antigen receptor (CAR) T-cell therapy and haploidentical hematopoietic stem-cell transplantation (HSCT) has shown promising results in patients with relapsed or refractory hematologic cancers. The approach is particularly beneficial for individuals who are not eligible for conventional allogeneic HSCT due to various reasons. The study, published in the New England Journal of Medicine, sheds light on a new potential treatment modality for these challenging cases.
The study included 10 patients with relapsed or refractory hematologic cancers, all of whom achieved complete remission after receiving CAR T-cell therapy. The majority of patients had minimal residual disease-negative complete remission, showcasing the effectiveness of this treatment approach. Following CAR T-cell therapy, nine patients underwent haploidentical HSCT, with six remaining in minimal residual disease-negative complete remission at a median follow-up of 15.1 months. The estimated 1-year overall survival rate was 68%, demonstrating the potential clinical benefit of this strategy.
The innovative procedure utilized allogeneic CD7 CAR T-cell therapy to create a conducive environment for successful allogeneic HSCT. By incorporating lymphodepletion prior to CAR T-cell infusion, the researchers were able to achieve GVHD control and maintain the persistence of CAR T cells, thereby paving the way for a novel treatment approach. This strategy holds promise for addressing the challenges associated with allogeneic HSCT and offers a potential solution for patients who are unfit for traditional transplantation methods.
The study’s findings have sparked interest in further exploration of this “all-in-one” approach in larger cohorts of patients. By considering the use of dual CAR T-cell constructs targeting multiple antigens and incorporating this strategy in newly diagnosed cases of CD7-positive acute myeloid leukemia, researchers are poised to advance the current treatment paradigms in hematologic cancers. The potential for long-term tumor elimination and reduced relapse risk makes this approach an attractive option for patients with poor prognoses.
The patients enrolled in the study had various hematologic malignancies, with a median age of 56.5 years and a history of extensive prior treatments. Despite the remarkable efficacy of the treatment strategy, a few adverse events were noted, including cytokine release syndrome (CRS) and graft-versus-host disease (GVHD). While the majority of these events were manageable, a few patients experienced serious complications such as septic shock and infections post-transplantation. These adverse events highlight the need for careful monitoring and management in patients undergoing this novel therapy.
The sequential approach of CAR T-cell therapy followed by haploidentical HSCT offers a promising treatment option for patients with relapsed or refractory hematologic cancers. The study’s results underscore the potential of this innovative strategy to improve outcomes in challenging cases and pave the way for future advancements in leukemia treatment. As researchers continue to explore the intricacies of this therapeutic approach, patients with hematologic malignancies hold hope for better and more effective treatment modalities.

Leave a Reply