Aging presents a complex relationship with cancer risk. Initially, individuals see an increase in the likelihood of developing cancer as they enter their 60s and 70s. This heightened risk can be attributed to the accumulation of genetic mutations over the decades. However, counterintuitively, research indicates that the risk of cancer begins to decline after reaching around 80 years of age. This phenomenon raises an intriguing question: what biological mechanisms are responsible for this apparent decline in cancer risk among the elderly? Recent studies shed light on this issue, revealing critical insights into lung cancer dynamics through their investigations into alveolar type 2 (AT2) stem cells.
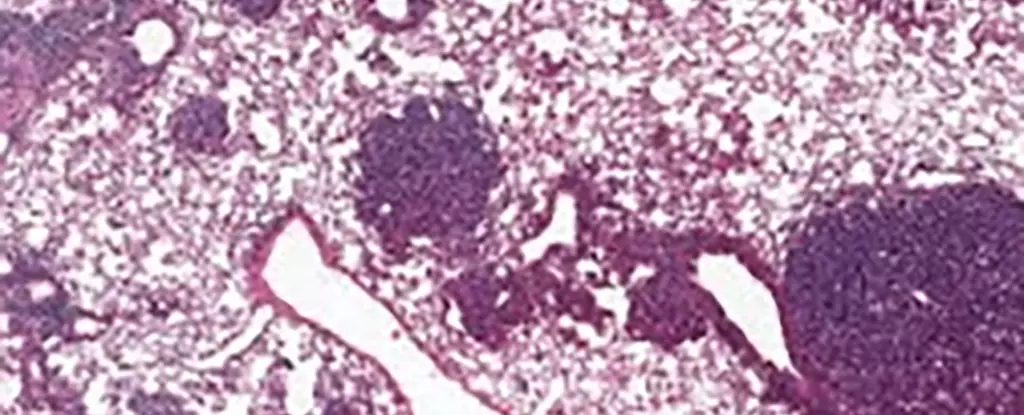
An international research team focused on understanding the behavior of AT2 stem cells, essential players in lung regeneration, and their connection to lung cancer. These stem cells are of particular importance because they are often implicated in the onset of lung cancers. The researchers observed a noteworthy increase in a protein known as NUPR1 in older mice. Elevated levels of NUPR1 seemed to induce a condition of functional iron deficiency within these cells, despite their actual iron content being relatively high. This disconnect between iron availability and cellular functionality led to decreased regenerative capabilities, effectively curtailing both healthy cell proliferation and the progression of cancerous tumors.
As noted by Xueqian Zhuang, a cancer biologist at Memorial Sloan Kettering Cancer Center (MSK), “Aging cells lose their capacity for renewal and therefore for the runaway growth that happens in cancer.” Thus, while aging cells appear to be equipped with necessary nutrients, their altered state hinders their capacity to function properly, which can ultimately limit the growth of cancer.
Compellingly, the mechanisms observed in mouse models also translated to human cells. The study found that increased NUPR1 activity corresponded with a decrease in iron availability for human cells as well. When researchers conducted interventions to artificially lower NUPR1 or increase iron levels, they noted a resurgence in cellular growth capabilities. These findings potentially pave the way for novel therapeutic strategies that could target iron metabolism, particularly in older populations, perhaps offering avenues to restore lung function in individuals suffering from prolonged consequences of respiratory illnesses like COVID-19.
Furthermore, this research opens avenues for deeper exploration into cancer treatment protocols that leverage ferroptosis— a unique form of cell death instigated by iron levels. Researchers discovered that older cells exhibited greater resistance to treatments based on ferroptosis due to their functional deficiencies in iron processing. Hence, interventions focusing on ferroptosis could become more effective if applied earlier in life, highlighting the importance of timely diagnosis and intervention in cancer therapy.
These findings prompt a reevaluation of our understanding of cancer prevention strategies. According to Tuomas Tammela, also associated with MSK, younger individuals are likely to face significantly higher cancer risks associated with lifestyle choices. This suggests that preventative measures aimed at reducing exposure to known carcinogens, such as smoking and excessive sun exposure, should be prioritized more than previously acknowledged.
Additionally, as this research underscores, cancer treatments must be customized to consider various factors, including the type and stage of cancer, the patient’s overall health, and their age. The notion of personalized medicine is becoming increasingly vital, and the findings regarding NUPR1 support the call for more individualized approaches in treating cancer.
Despite the significant progress represented by these findings, key questions remain unanswered. Notably, the intricate connection between aging, NUPR1 function, and stem cell activity necessitates further investigation. As Zhuang states, “There’s still a lot that’s unknown about how aging actually changes the biology of cancer.” Future research must delve deeper into these complex interactions, enabling us to develop more effective strategies for cancer treatment and prevention across different ages, thus ultimately advancing our understanding of cancer biology throughout the human lifespan.

Leave a Reply