For decades, scientists viewed glycogen in the brain primarily as an energy reserve, a backup system for neurons when immediate glucose supplies ran low. This outdated perspective limited the scope of neurological research, inadvertently overlooking a potentially pivotal player in brain health. Now, emerging evidence suggests that glycogen’s role extends far beyond passive storage; it is actively involved in the development of neurodegenerative diseases such as Alzheimer’s. This paradigm shift demands attention, as it opens avenues for innovative treatments rooted in metabolic modulation—a bold move away from traditional approaches that largely targeted protein accumulations or neuroinflammation.
Glycogen and Tau: An Intricate, Dangerous Dance
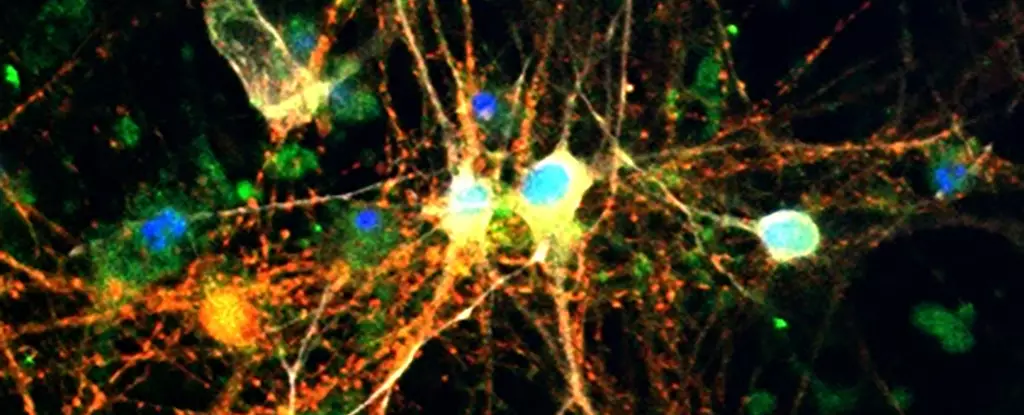
The new findings reveal a disturbing interaction between tau proteins—known culprits in Alzheimer’s—and glycogen, which is stored and metabolized within neurons. Scientists observed elevated glycogen levels in models of tauopathy and in human brains affected by Alzheimer’s. This suggests that glycogen accumulation might not be merely a symptom but could actively contribute to neuronal damage. The mechanism appears to involve tau-induced impairment of glycogen breakdown, leading to a vicious cycle of buildup. As glycogen accumulates abnormally, it may interfere with neuronal functions, impairing cell signaling and magnifying oxidative stress, thus fueling neurodegeneration.
This relationship is troubling because it challenges the longstanding notion that tau pathology is solely about protein misfolding and aggregation. Instead, it proposes that metabolic disturbances—specifically, glycogen dysregulation—may be central to disease progression. Such an insight shifts the narrative, emphasizing the importance of brain metabolism in maintaining neuronal integrity.
Targeting Glycogen Metabolism: An Unexplored Frontier
One of the most encouraging aspects of this research is the identification of glycogen phosphorylase (GlyP), the enzyme responsible for breaking down glycogen, as a therapeutic target. Experimental boosting of GlyP activity in fruit fly models led to improved clearance of glycogen, reduced oxidative stress, and even an increase in lifespan of models with tauopathy. These results suggest that restoring proper glycogen metabolism can bolster neuronal defenses and possibly slow or halt disease progression.
Furthermore, dietary interventions, such as low-protein diets, demonstrated remarkable effects. When tau-affected flies adhered to such diets, they experienced longer lifespans and less brain damage, indicating that metabolic shifts can be harnessed to combat neurodegeneration. The addition of pharmacological agents mimicking dietary restriction effects further solidifies this concept. Drugs based on molecules like 8-Br-cAMP showed promise, hinting at the possibility of developing metabolic therapies tailored to modify glycogen dynamics in humans.
Implications for Future Treatments and Broader Impact
These breakthroughs herald a potential overhaul in how we approach neurodegenerative diseases. Instead of solely focusing on amyloid plaques or tau tangles, future strategies might incorporate metabolic modulation—aiming to normalize glycogen levels and enhance enzymatic breakdown. Interestingly, existing medications such as GLP-1 receptor agonists, currently used to treat diabetes, are being investigated for their neuroprotective effects. Their apparent interaction with glycogen pathways could revolutionize treatment protocols, making existing drugs more versatile and repurposing them for cognitive health.
However, the road ahead is fraught with challenges. Translating findings from fruit flies and animal models to human therapies requires caution and further research. The complexity of glucose metabolism, neuronal diversity, and individual variability means that a one-size-fits-all solution is unlikely. Nevertheless, the paradigm has shifted: brain glycogen is no longer a passive storage molecule but an active, potentially manipulable component of neuronal health and disease.
Critically, this new perspective bridges the gap between metabolism and neurodegeneration, emphasizing the need for a more holistic understanding of brain aging. It underscores that neurodegenerative diseases are not solely about genetic or protein factors but involve deeper metabolic networks that can be targeted for intervention. As research advances, we may see a future where preventing glycogen dysregulation becomes a standard component of neuroprotective strategies, ultimately transforming the landscape of neurodegenerative disease management.

Leave a Reply