In recent discussions surrounding the ongoing NHS strike turmoil, it’s tempting to see the political landscape through a lens of strategic positioning and administrative maneuvering. Yet, beneath this veneer lies a deeper—and far more troubling—disconnect between leadership and frontline workers. On the surface, the engagement of figures like Wes Streeting might seem driven by a genuine desire to uphold healthcare services, but a closer examination reveals a fundamental failure: a lack of understanding, or perhaps a willful blindness, to the realities faced by resident doctors. The optimism that accompanies ambitions of reform and 10-year plans often obscures the fragile, volatile interplay of trust and unmet needs among those who deliver care. This disconnect is symptomatic of a broader cultural issue within the NHS—an institution seemingly more committed to grand strategy than addressing its most urgent internal crises.
Pay Disputes and the Erosion of Morale
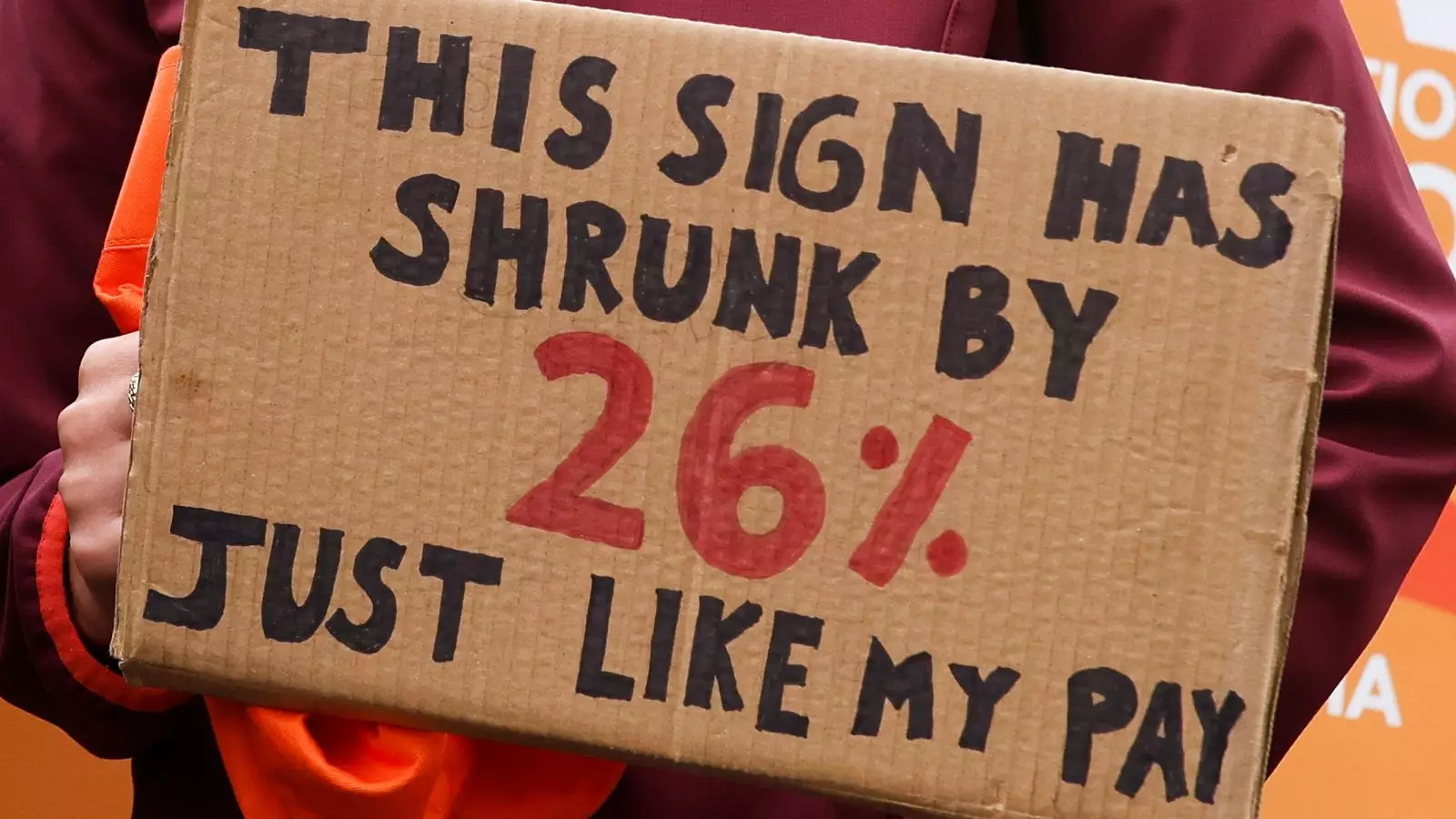
The core issue fueling these strikes, as always, revolves around pay: a seemingly straightforward matter that grows increasingly complex in the context of the NHS’s long-term sustainability. Resident doctors, whose labor is critical to the system’s functioning, have been vocally demanding a 26% pay restoration—an assertion rooted in years of perceived underpayment. Their advocate, the BMA, frames this as an imperative correction for 17 years of erosion, highlighting how wage stagnation fuels burnout, attrition, and a dangerous decline in quality care. Yet, the government counters with figures indicating physicians received a nearly 29% pay increase recently, creating a paradox that fuels public skepticism. This standoff exposes a crucial failure: attempts at balancing fiscal responsibility with workforce well-being are mired in miscommunication, misinformation, and a loss of empathy. It demonstrates how political narratives often distort the real human toll behind the statistics, undermining trust and fueling the cycle of dissatisfaction.
Strategic Failures and the Myth of Local Autonomy
In response to the strikes, there has been a push for decentralized decision-making—trust leaders, it is argued, know their staff and patients better, so they should be empowered to make operational choices during crises. But this concept assumes an adequately prepared, well-resourced management structure capable of managing chaos—a premise that is painfully optimistic. In reality, such a decentralization risks creating a patchwork of inconsistent policies, and with staff shortages already endemic, it threatens to undermine the essential safety net that patient care depends on. Allowing local discretion without substantial support risks turning the NHS into a fragmented system where quality and safety become casualties of political expediency. The government’s reliance on this narrative of local empowerment glosses over the systemic underfunding and staffing crises that make such measures merely band-aids rather than solutions.
The Political Theater and the Loss of Moral Clarity
Politicians and healthcare leaders seem more focused on pinning blame than addressing the root causes of the crisis. The exchange of accusations—blaming each other for putting patients at risk—does little to solve these deep-seated issues. Instead, it fosters a toxic environment where public trust wanes, and the moral authority of the healthcare system diminishes. When decisions are framed primarily in terms of political survival or optics, it becomes nearly impossible to enact meaningful change. The core problem is not just about pay or resource allocation but also about the values that underpin this public institution—values of fairness, respect, and the recognition of frontline workers’ indispensable contributions. Without a sincere prioritization of these principles, the NHS risks becoming emboldened as a symbol of bureaucratic neglect, further alienating the very people tasked with delivering care and the public that depends on it.
A Center-Left Perspective on Needs and Realities
From a center-wing liberal standpoint, the essential failure lies in the inability to strike a fair compromise that recognizes both fiscal limits and the undeniable demand for fair treatment of NHS staff. There is an urgent need to shift from short-term political posturing to long-term strategic investment—investing in staff wages, mental health support, and systemic reform that truly values and sustains the workforce. The NHS’s future depends on restoring a sense of moral reciprocity: respecting the dedication of resident doctors by addressing their pay and working conditions comprehensively, rather than resorting to tactical compromises that exacerbate distrust. If the government and NHS leadership fail to see beyond the immediate headlines to the fundamental human needs of their staff, they risk endangering the very fabric of the nation’s healthcare system. In the end, sustainable reform hinges on genuine recognition, fairness, and demonstrating that the NHS values its front line just as much as its strategic ambitions.

Leave a Reply