Selective serotonin reuptake inhibitors (SSRIs) have become a cornerstone in the treatment of mood disorders, particularly depression and anxiety. With millions of prescriptions issued annually, these medications offer hope for relief from debilitating symptoms. However, the usage of SSRIs comes with a cloud of controversy, primarily due to the ambiguities surrounding their long-term efficacy and mechanisms of action. This article delves into a comprehensive study led by psychologist Vibeke Dam from Copenhagen University that elucidates the cognitive ramifications of SSRIs, providing insights into how these drugs may not only influence mood but also cognitive functions.
In a thoughtful exploration of SSRIs’ cognitive effects, Dam and her research team evaluated 90 patients diagnosed with moderate to severe depression. The study employed brain imaging techniques alongside cognitive assessments to track changes over an eight-week period while patients were administered the SSRI escitalopram. Initial evaluations assessed both cognitive function and mood before the commencement of treatment, allowing for a baseline against which to measure change. At the end of the treatment period, brain scans were conducted again on a subset of 40 patients, and further cognitive assessments followed at week 12.
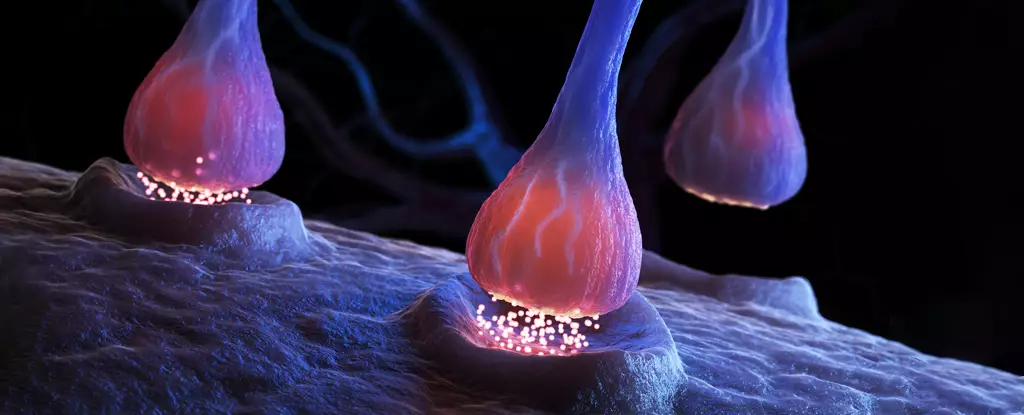
Interestingly, the results indicated a nearly 10 percent decrease in serotonin receptor binding post-treatment, which raises questions regarding the traditional understanding of SSRIs as mere serotonin boosters. Particularly noteworthy was the correlation between cognitive improvements—specifically in verbal memory—and the changes in receptor binding. The patients showing the least change in the 5HT4 serotonin receptor exhibited the most significant improvements in memory, suggesting a complex relationship that may transcend simplistic serotonin replenishment.
The findings highlight the pivotal role of the 5HT4 receptor in cognitive improvement amongst participants. Dam’s assertion that direct stimulation of this specific receptor could provide a potential target for optimizing antidepressant outcomes opens new avenues for understanding SSRIs. This receptor has often been overlooked in discussions surrounding SSRIs, yet its importance in cognitive functions related to mood disorders cannot be understated.
Historical data from Dam’s previous studies indicate that unmedicated patients suffering from major depressive disorder possess a lower density of these receptors compared to healthy individuals. This raises intriguing questions about the relationship between cognitive deficits and depression, propelling us closer to understanding how SSRIs functionality may not solely hinge on mood enhancement but also cognitive restoration.
While the results provide substantial insights, the study also identifies critical limitations. Ethical constraints precluded the inclusion of a placebo group, adding a layer of uncertainty regarding the observed improvements. Without a control group, it’s challenging to ascertain whether the positive cognitive outcomes were directly attributable to the SSRI treatment or due to other factors that remain unaccounted for.
Moreover, while patients exhibited noticeable improvements in some cognitive functions, the disconnect between these cognitive enhancements and mood improvements casts doubt on the efficacy of SSRIs as straightforward treatment options for depression. Even as the hypothesis regarding 5HT4 receptors gains traction, the overarching question remains: do SSRIs genuinely assist in alleviating the core symptoms of depression?
The landscape of antidepressant research is rife with complexities, especially as recent studies have begun to challenge the very premise that SSRIs provide greater benefit than a placebo. This paradigm shift in understanding makes it increasingly essential for researchers and clinicians alike to explore alternative methods for diagnosing and treating depression, particularly those that focus on cognitive functions. Dam and her colleagues emphasize the need for further investigation into the mechanisms underpinning both SSRIs and alternative therapies, thereby fostering an environment of precision psychiatry.
As the research community strives to unravel the nuances of cognitive impairments in depression, a crucial takeaway is the importance of safeguarding patients. While SSRIs remain a common denominator in mood disorder treatment, discontinuation without professional guidance can lead to adverse side effects. Consequently, ongoing research into the multifaceted mechanisms of SSRIs is vital in preserving patient safety and enhancing treatment efficacy.
The study conducted by Vibeke Dam and her team broadens the discourse around SSRIs by linking them to cognitive changes, highlighting the critical role of the 5HT4 receptor. As we seek to deepen our understanding of mood disorders and the effects of medications like SSRIs, the research presents an opportunity to refine treatment strategies, ensuring that patients receive the most effective and nuanced care possible. Future studies will be essential in shedding light on these mechanisms, with the ultimate goal of optimizing therapies for those navigating the complexities of depression.

Leave a Reply