Chronic inflammatory demyelinating polyneuropathy (CIDP) is a disease that is often misdiagnosed or diagnosed late due to its complexity and rarity. Standard treatments like intravenous immunoglobulin (IVIG), steroids, and plasma exchange are not always effective, especially in certain CIDP phenotypes. To improve both diagnosis and treatment outcomes, valid biomarkers are crucial. However, CIDP lacks widely accepted measures for biomarkers, making it challenging to manage the disease effectively. According to Jeffrey Allen, MD, from the University of Minnesota, biomarkers are needed to enhance the accuracy of diagnosis and to gain a better understanding of disease activity and treatment responses.
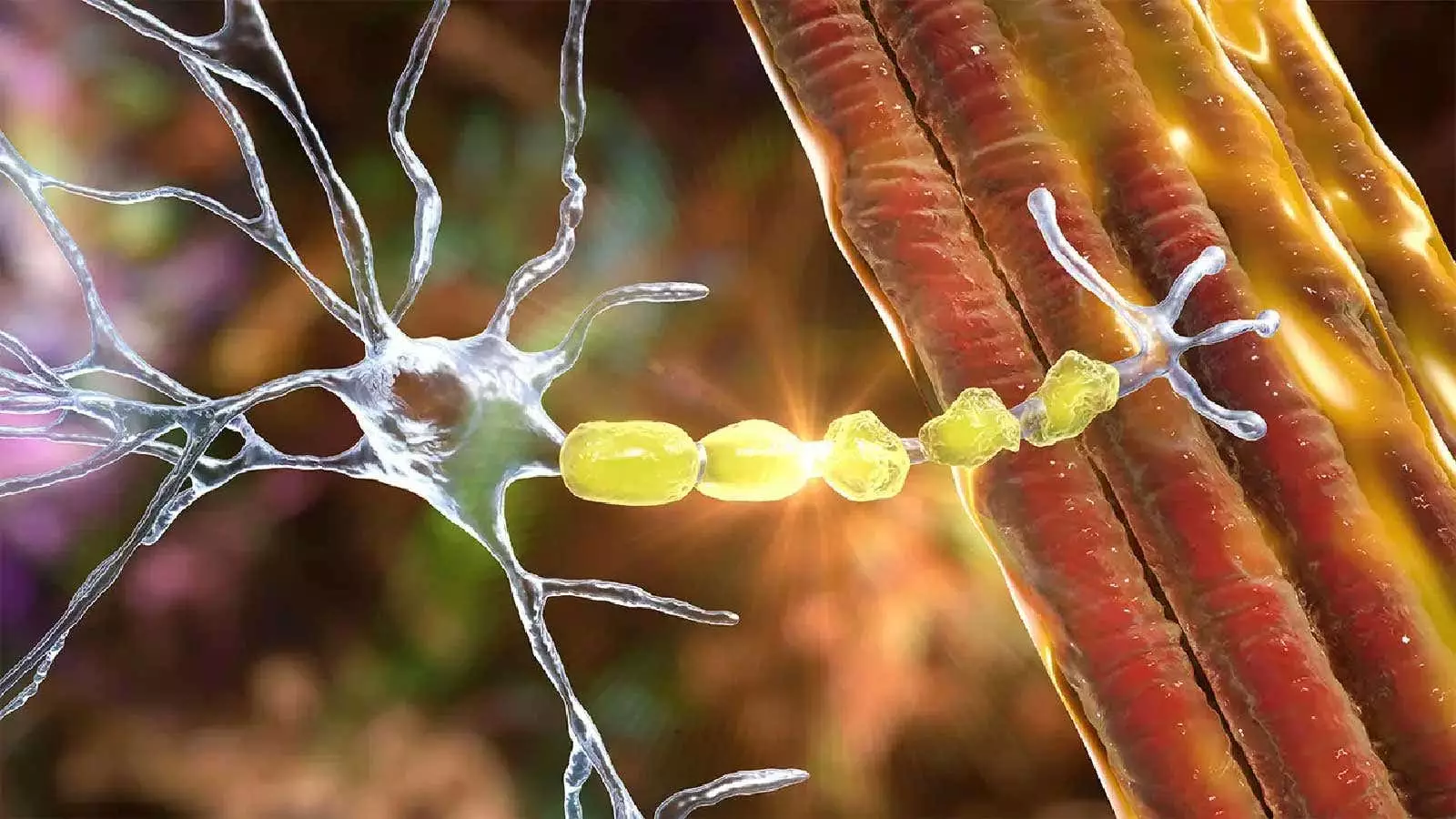
Recent studies have explored various potential biomarkers for CIDP, including autoantibodies, cytokines, complement proteins, and immunoglobulin G (IgG) levels. However, due to the heterogeneity of CIDP, a combination of biomarkers that can reflect nerve integrity, treatment effects, and immune system activity may be necessary. For instance, serum neurofilament light chain (NfL) has shown promise as a biomarker for disease activity, particularly in patients starting induction treatment. Elevated levels of serum NfL have been linked to disease progression, highlighting its potential as an indicator of CIDP severity. Additionally, autoimmune nodopathies in CIDP patients have shown resistance to IVIG therapy, suggesting that certain antibodies like anti-neurofascin-155 and anti-contactin-1 could serve as biomarkers for treatment response.
Ongoing studies such as the INCbase project aim to identify new biomarkers for CIDP by collecting biosamples from a diverse group of patients with the disease. Imaging techniques like magnetic resonance neurography (MRN) have also shown promise in assessing nerve damage in CIDP. MRN provides detailed images of nerve continuity and integrity, offering a non-invasive alternative to traditional nerve conduction studies and electromyography. Whole-body MRN has been able to detect pathological changes in nerve structures of CIDP patients, emphasizing the importance of imaging biomarkers in improving diagnostic accuracy.
While nerve conduction studies and electromyography are currently the primary methods for CIDP diagnosis, they have limitations in terms of discomfort for patients and insufficient visualization of nerve anatomy. Ultrasound imaging has emerged as a valuable tool for distinguishing immune neuropathies like CIDP from other conditions. High-frequency ultrasound of nerve structures has shown potential in differentiating CIDP from controls, providing a non-invasive and accurate method for diagnosis. The use of ultrasound and MRI in CIDP diagnosis has been recommended in recent guidelines to improve diagnostic certainty in patients meeting CIDP criteria.
Moving forward, more research is needed to identify novel biomarkers that can aid in the diagnosis and treatment of CIDP. By understanding the complex mechanisms underlying the disease and exploring a combination of biomarkers, healthcare providers can better tailor treatment strategies for individual patients. With advancements in imaging technology and ongoing studies like INCbase, the future looks promising for the development of effective biomarkers for CIDP. Increased collaboration among researchers and clinicians will be essential in accelerating the discovery of reliable biomarkers for this debilitating neurological disorder.

Leave a Reply