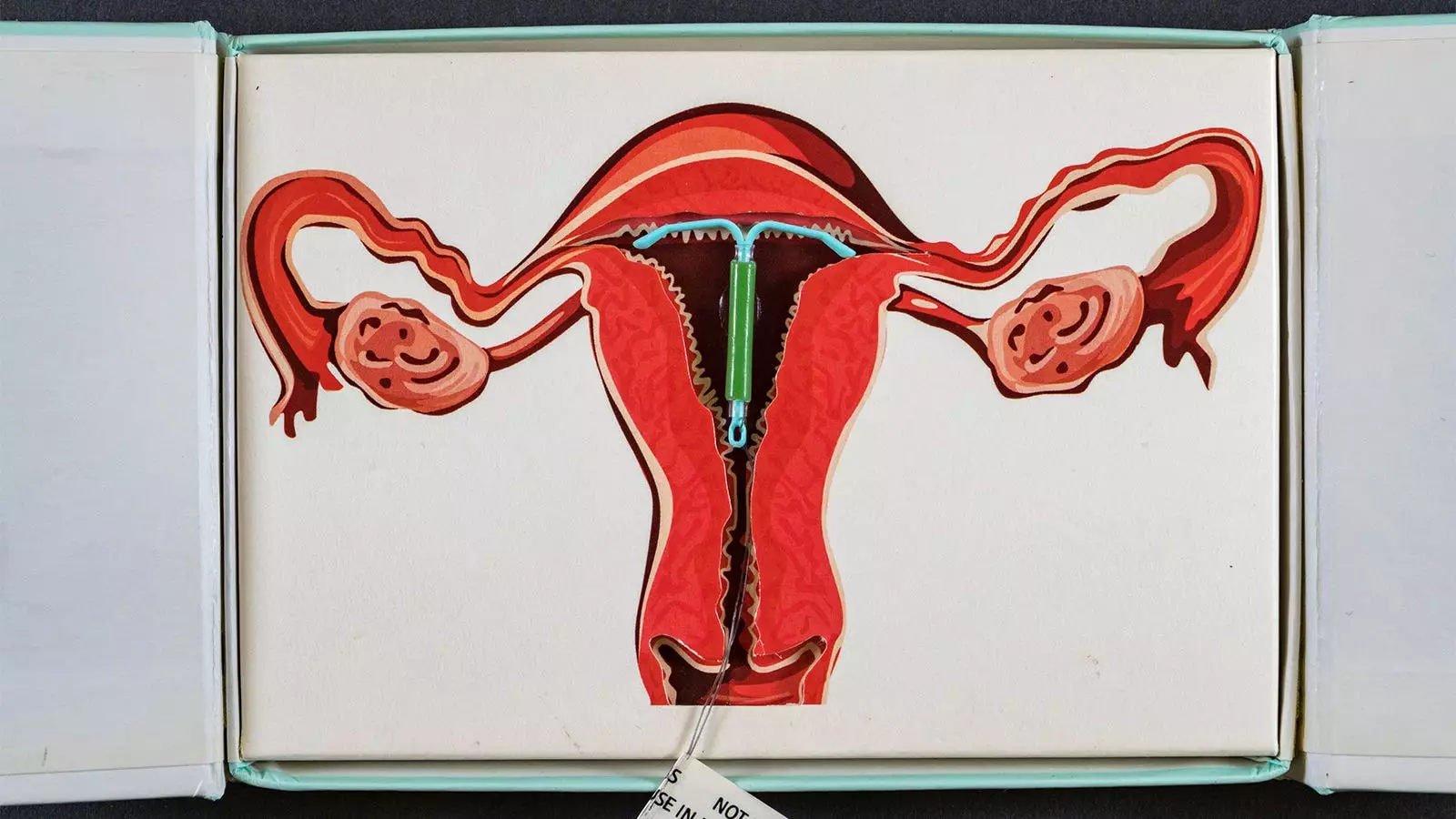
Recent research from Denmark has sparked significant discussions regarding the potential health risks associated with hormonal contraceptive methods, specifically focusing on the levonorgestrel-releasing intrauterine device (IUD). This study highlights the alarming statistical correlation between the use of these devices and an increased risk of breast cancer in women under the age of 50. Throughout this article, we shall delve into the study’s findings, implications, and the critical need for informed discussions surrounding contraceptive choices.
The Danish registry study, comprising nearly seven years of follow-up data, involved a comprehensive analysis of 78,595 women using levonorgestrel-releasing IUDs compared to an equal number of non-users of hormonal contraceptives. This quasi-experimental design aimed to shed light on the long-term risks associated with IUD use—an area that has not been sufficiently explored in previous literature. The average age of participants was 38 years, allowing researchers to evaluate a demographic potentially at risk for breast cancer.
One of the most striking findings was the relative increase in breast cancer diagnoses. Women utilizing levonorgestrel-releasing IUDs faced a 40% higher likelihood of receiving a breast cancer diagnosis compared to their non-user counterparts. Moreover, this risk escalated with the duration of IUD usage, peaking at an 80% increased risk in those who reported using the device for 10-15 years.
The results indicated 1,617 new breast cancer cases, with 720 occurring in users of the IUD. While the calculated hazard ratios provided critical insights—1.4 for LNG-IUS users versus non-users—the trend’s statistical significance remained elusive, evidenced by a P-value of 0.15. This highlights an often overlooked issue in medical research: statistical significance doesn’t always equate to clinical relevance, and the need for a more granular analysis is paramount.
Moreover, the data suggested notable excess breast cancer diagnoses, with varying rates identified based on the duration of IUD use. While the findings establish a correlative link between longer usage and higher risks, they ought to be interpreted with caution considering other potential confounding factors, such as personal medical histories and the interaction with other hormonal contraceptives.
The current study builds upon previous research wherein a similar risk association was noted, albeit without distinguishing between various hormonal contraceptive methods. It also aligns with findings from other studies indicating an increased risk for demographic groups predisposed to breast cancer, such as BRCA1 gene carriers. Understanding the layered risks associated with hormonal contraceptives is essential for informed healthcare choices.
Crucially, patients and healthcare providers must engage in comprehensive discussions concerning the merits and risks associated with these contraceptive methods. The statistical findings raise an urgent call for the inclusion of breast cancer risk information in counseling practices regarding IUD usage, especially given the growing trend of hormonal contraceptive use among younger women.
Concluding Thoughts
The Danish study contributes to an essential dialogue regarding the long-term health implications of hormonal contraceptives, specifically levonorgestrel-releasing IUDs. With statistics indicating a significant breast cancer risk associated with prolonged usage, it is imperative that women are fully informed about their choices. The healthcare community must take proactive steps to ensure that all users understand the potential long-term risks related to their contraceptive decisions. Ultimately, more extensive longitudinal studies are warranted to elucidate the complexities of hormonal contraceptives and their implications on women’s health. Addressing these issues is crucial for shaping safer contraceptive policies and practices in the future.

Leave a Reply