The landscape of medical treatment for obesity is undergoing significant transformation, especially with the recent acknowledgment by Medicare that Eli Lilly’s new obesity drug, Zepbound, will now be covered for obstructive sleep apnea (OSA) patients. This development is pivotal not only for those already struggling with obesity and associated sleep disorders but also for the broader healthcare system, which continues to grapple with the soaring rates of obesity-related health issues.
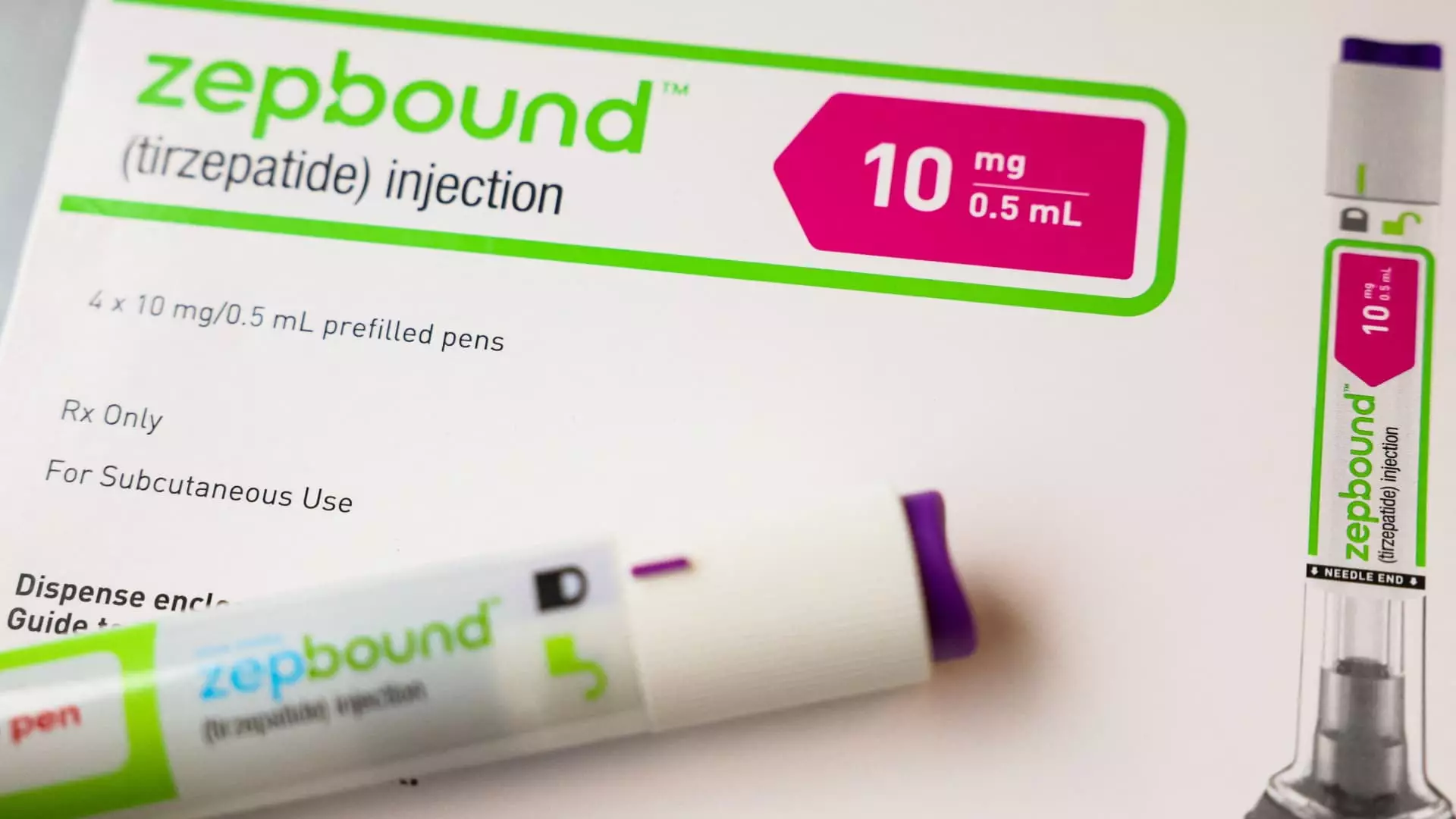
Zepbound has quickly emerged as a frontrunner in obesity-related treatments, garnering substantial demand despite its steep price point of approximately $1,000 before insurance coverage. The drug’s recent approval by the Food and Drug Administration (FDA) for the treatment of moderate-to-severe OSA indicates a significant leap in the recognition of obesity as a multifaceted condition that warrants comprehensive therapeutic strategies. This underscores the fact that effective management of obesity is critical not only for weight reduction but also for mitigating serious comorbidities like OSA, which affects millions of Americans.
Until now, Medicare, along with many private insurers, had been reticent to cover obesity medications, primarily due to stringent regulations governing drug approvals and usage. However, the Centers for Medicare & Medicaid Services (CMS) have stipulated that Zepbound can be included in Medicare Part D plans if its usage aligns with FDA-approved indications beyond mere weight loss. This stipulation explores the intersectionality of obesity treatment and the pressing need for better sleep health among affected populations.
Despite this significant breakthrough, challenges remain surrounding the accessibility of Zepbound and similar drugs through insurance plans. Medicare Part D plans might implement prior authorization requirements to guarantee that prescribing physicians justify the need for Zepbound based on its prescribed uses for OSA. This process can impose additional barriers for patients, delaying access to necessary treatments and complicating interactions between healthcare providers and insurers.
Moreover, the matter of state Medicaid programs adds another layer of complexity. Coverage decisions hinge on the conditions for which Zepbound is prescribed, along with whether Eli Lilly has entered into Medicaid rebate agreements—a critical factor that determines if the drug will be accessible to low-income patients. As it stands, state Medicaid is obligated to cover Zepbound only if prescribed for OSA; should it be prescribed solely for weight loss, coverage is not guaranteed. This raises important concerns regarding equity in healthcare access, particularly for vulnerable populations who face both financial and health-related challenges.
The Biden administration’s proposal to expand Medicare and Medicaid coverage for obesity medications marks a noteworthy potential evolution in healthcare policy. If implemented, this move would open the door for millions suffering from obesity-related conditions to access effective pharmacotherapies such as Zepbound, with estimated costs reaching up to $35 billion over the next decade. While critics may raise alarms about the financial implications, proponents argue that investing in preventive health measures may ultimately lessen the economic burden associated with obesity-related diseases.
The dynamic between pharmaceutical companies like Eli Lilly and Novo Nordisk, which are actively researching additional potential uses for their weight loss drugs, illustrates the rapidly evolving field of obesity treatment. As clinical trials for uses beyond weight management, such as addressing chronic kidney disease and fatty liver disease, yield results, the possibility for broader drug coverage stands to reshape patient care strategies in the United States.
The inclusion of Zepbound under Medicare drug plans signifies a noteworthy shift towards recognizing the importance of treating obesity not just as a standalone condition but as part of a larger tapestry of health issues, including obstructive sleep apnea. Although barriers exist, particularly in terms of insurance coverage and regulatory requirements, the potential benefits highlight the urgent need for comprehensive approaches to obesity treatment. As society continues to grapple with this epidemic, innovative solutions and policy changes will be crucial in fostering better health outcomes and improving quality of life for millions across the country.

Leave a Reply