Axial spondyloarthritis (axSpA) is a complex and often debilitating form of spondyloarthritis that primarily impacts the spine and sacroiliac joints. Patients suffering from this condition experience significant pain and stiffness, which can severely affect mobility and the quality of life. The disease manifests in two major forms: radiographic axSpA, also known as ankylosing spondylitis, and non-radiographic axSpA. Despite both types sharing similar clinical characteristics and challenges in treatment, they present unique management issues that affect patient care and outcomes.
In the management of axSpA, it has been established that treatment efforts must be multidisciplinary, combining pharmacological and non-pharmacological strategies to optimize patient outcomes. With the primary goal of alleviating pain and hindering disease progression, the treatment landscape has evolved significantly, especially for patients who are unresponsive to traditional nonsteroidal anti-inflammatory drugs (NSAIDs).
According to the latest guidelines from the Assessment of SpondyloArthritis International Society and the European League Against Rheumatism (ASAS-EULAR), the first line of treatment for axSpA typically involves NSAIDs. For certain patients, especially where peripheral joints are involved, disease-modifying agents like sulfasalazine can be introduced. Nevertheless, not all patients find relief with NSAIDs; thus, the introduction of additional therapeutic options is critical.
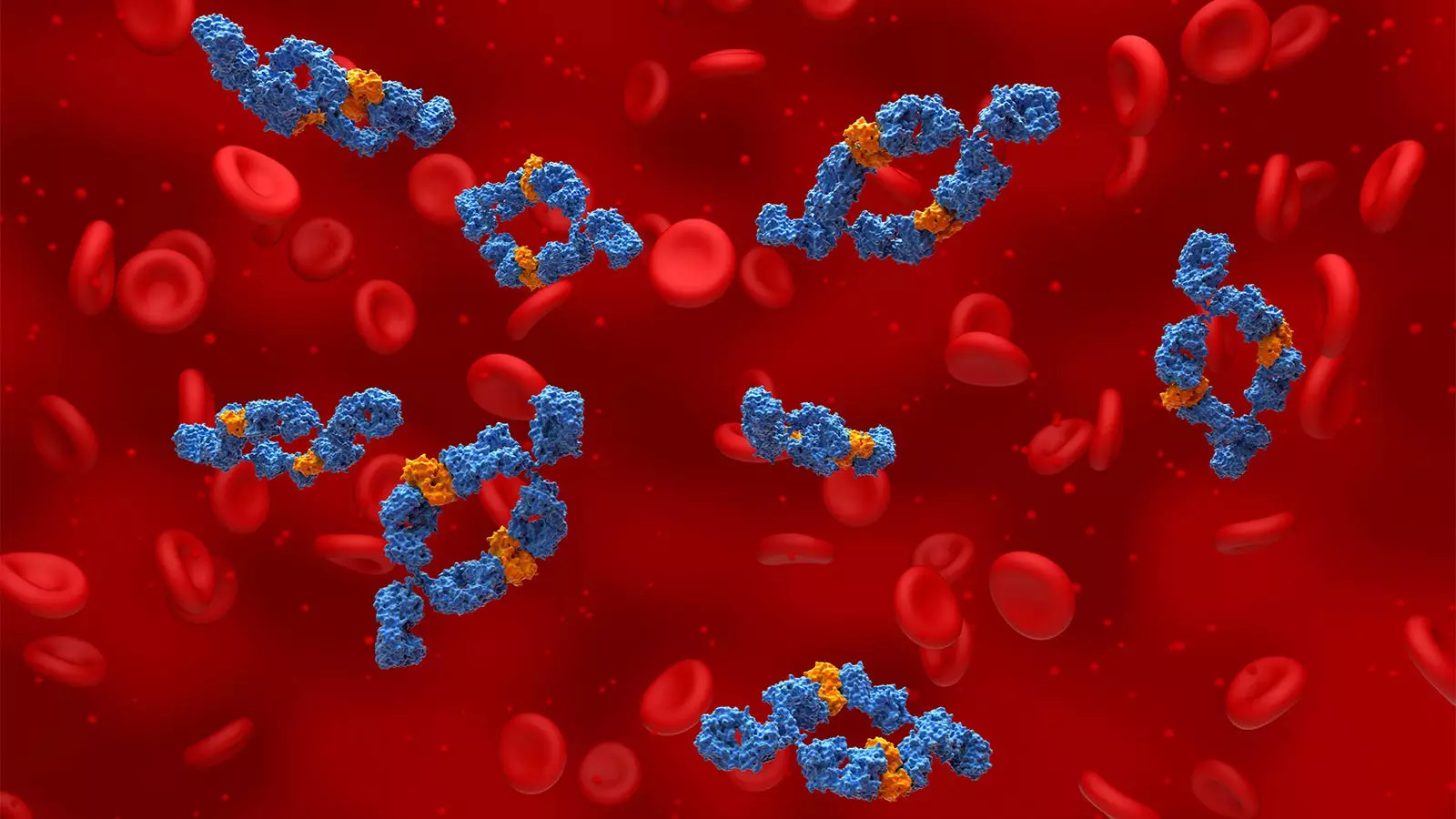
The landscape for axSpA treatment is diversifying, with innovative biological agents entering the field. In particular, tumor necrosis factor (TNF) inhibitors and monoclonal antibodies targeting interleukin (IL)-17 have garnered significant attention. Moreover, Janus kinase (JAK) inhibitors have been introduced as viable options for certain patient profiles. The recent FDA approval of bimekizumab—a monoclonal antibody that inhibits both IL-17A and IL-17F—marks a promising advancement. This agent has shown efficacy in treating both non-radiographic and radiographic axSpA.
Recent clinical trials, specifically the BE-MOBILE 1 and BE-MOBILE 2 studies, have generated compelling evidence for the effectiveness of bimekizumab. These trials indicate a remarkable response rate of around 45% at the primary endpoint measurement for patients treated with the drug, which highlights its potential as a significant addition to current treatment paradigms. In contrast, the response rates for placebo recipients were markedly lower, emphasizing the drug’s efficacy.
However, while the success of bimekizumab is certainly encouraging, questions remain about its comparative effectiveness vis-à-vis existing therapies. Experts, including Dr. Atul Deodhar from Oregon Health and Science University, have highlighted the need for further studies to draw definitive conclusions regarding its superiority over existing treatments. The lack of head-to-head clinical trials leaves much uncertainty, particularly regarding whether dual blockade of IL-17A and IL-17F is more effective than targeted inhibition of IL-17A alone.
The choice of therapy often hinges on the clinical nuances of each patient, including the presence or absence of extra-articular manifestations. Dr. Eric Toussirot elaborates that while TNF inhibitors remain popular choices, the integration of JAK inhibitors has provided more options, albeit with specific cardiovascular restrictions. The available TNF inhibitors—such as adalimumab and infliximab—alongside IL-17 agents like secukinumab and ixekizumab, offer a range of therapeutic avenues.
A significant observation from recent studies highlights the challenges associated with JAK inhibitors; they exhibit higher discontinuation rates in comparison to TNF and IL-17 inhibitors. This phenomenon is noteworthy as it underscores the need to consider patient profiles more stringently before initiating therapy with these agents.
Despite the promising advancements in treatment, the journey for axSpA patients remains fraught with challenges. The arrival of bimekizumab in the therapeutic pipeline offers hope, but further comparative research is crucial to validate its position within the standard treatment framework. Additionally, continued evaluation of patient response rates and side effects for all treatment classes will be essential.
While the evolving landscape of axSpA therapy presents newfound opportunities for improving patient outcomes, clinicians must remain vigilant in monitoring patients’ responses and adjusting treatment protocols as needed. The path forward necessitates a collaborative and informed approach to ensure that the best possible outcomes are achieved for individuals grappling with this complex condition.

Leave a Reply