The recent breakthroughs at Duke University are nothing short of revolutionary, yet undeniably controversial. Surgeons successfully revived a ‘dead’ heart—one that had ceased beating for over five minutes—only to transplant it into a vulnerable infant. The unprecedented feat underscores the limitless potential of biomedical science but also exposes fundamental conflicts within ethical boundaries. The success stories imbue hope into a system desperately in need of expansion but simultaneously cast a spotlight on the murky moral waters surrounding the reanimation of human organs. Such advances threaten to redefine what we perceive as death, challenging long-held medical and ethical standards.
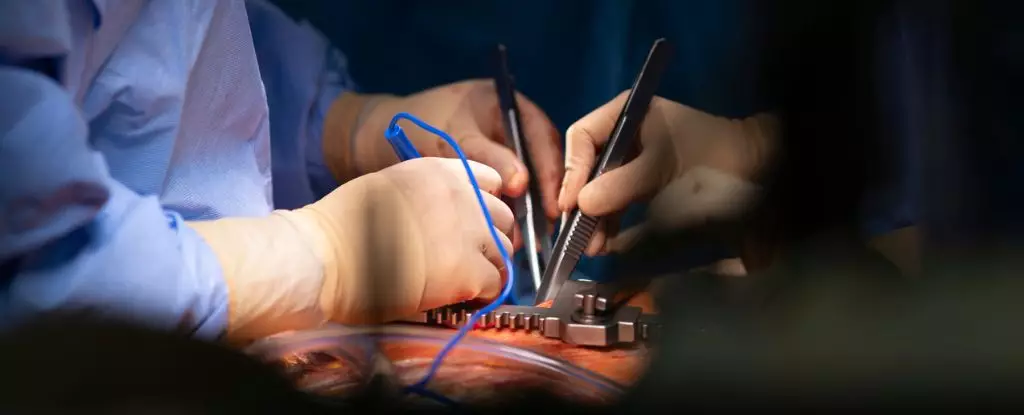
Efforts to resuscitate organs outside the traditional confines of circulation have unveiled a new frontier in transplantation medicine. The Duke team used specialized equipment—an oxygenator, centrifugal pump, and custom-designed reservoirs—to revive a tiny infant heart on the operating table. This procedure, a stark departure from conventional protocols, signifies a paradigm shift: instead of waiting for a donor to reach brain death, scientists are exploring ways to revive and preserve tissues more effectively. The possibility of extending the window for transplantation by reanimating hearts outside the body promises to remedy a pressing shortage—up to 20 percent of pediatric patients die on waiting lists primarily due to the organ scarcity.
However, this scientific triumph isn’t just a tale of progress; it is also a window into the complex ethical labyrinth that confronts modern medicine. While supporters argue that on-table reanimation could significantly broaden the donor pool, critics warn that it muddles the essential moral distinctions about defining death. If a heart is restarted after life support withdrawal, does that still count as death? The crux of the problem lies in the ambiguity—do we prioritize technological possibility over the human rights and dignity of the donor? The underlying concern is whether such practices risk trivializing death itself, transforming it into a reversible state that could be manipulated for medical gains.
Ethical Controversies and Moral Quandaries
The debate at the core of these revolutionary techniques hinges on uncomfortable questions: Should the potential to save more lives justify crossing moral lines? The United States currently relies heavily on brain death criteria to approve organ donation, but innovations like Duke’s on-table reanimation challenge this framework profoundly. Critics argue that reanimating a heart post-circulatory death blurs the line, effectively erasing the clear boundary that separates life from death. The heart, once considered the seat of life, now becomes a target for scientific rethinking, risking a dangerous normalization of circumventing established ethical standards.
Another contentious issue is the process of declaring death itself. In traditional protocols, death is unambiguous—when the brain ceases functioning, death is declared. But the ability to restart an organ after cessation of circulation cuts to the core of what constitutes true death. Are we venturing into a morally gray zone where death becomes a reversible event rather than a definitive endpoint? Such dilemmas threaten to diminish public trust and could foster a slippery slope toward commodification of human organs, where scientific possibility overtakes ethical integrity.
Meanwhile, Vanderbilt University offers an alternative that skirts these moral pitfalls. Their method involves preserving donor hearts using a cold-preserving flush without attempting to reanimate the organ prematurely. This approach maintains a necessary separation from the donor’s brain, thus sidestepping key ethical concerns. The evidence from initial procedures suggests that such preservation techniques could still significantly expand the donor pool without the contentious practice of reanimation. This less invasive approach might represent a more ethically sound pathway forward—balancing innovation with respect for human dignity.
Balancing Science and Morality in the Modern Era
As these technologies evolve, they force us to confront the uncomfortable reality: progress in medicine often marches ahead of ethical consensus. It is tempting to celebrate technological breakthroughs as the pinnacle of human ingenuity, yet it is equally vital to scrutinize whether such advancements respect our moral boundaries. The idea of reanimating a heart after death challenges fundamental notions of mortality—questions that society must answer collectively, not merely through the lens of scientific possibility.
Center-wing liberalism must serve as a guiding compass in this discourse, advocating for responsible innovation that promotes human rights and ethical integrity. While the urgency to save pediatric lives is apparent and compelling, it cannot come at the expense of eroding the moral principles that uphold human dignity. A careful, nuanced approach—favoring preserving organs without risking the moral chaos of reversible death—appears to be the most prudent course.
The future of organ transplantation hinges on a delicate interplay between groundbreaking science and steadfast ethical standards. It is crucial that we do not allow the pursuit of life-saving solutions to diminish the meaning of death or to devalue human life in the process. Responsible innovation must strike a balance—embracing new techniques that expand hope without compromising the moral fabric that safeguards societal trust and human rights.

Leave a Reply