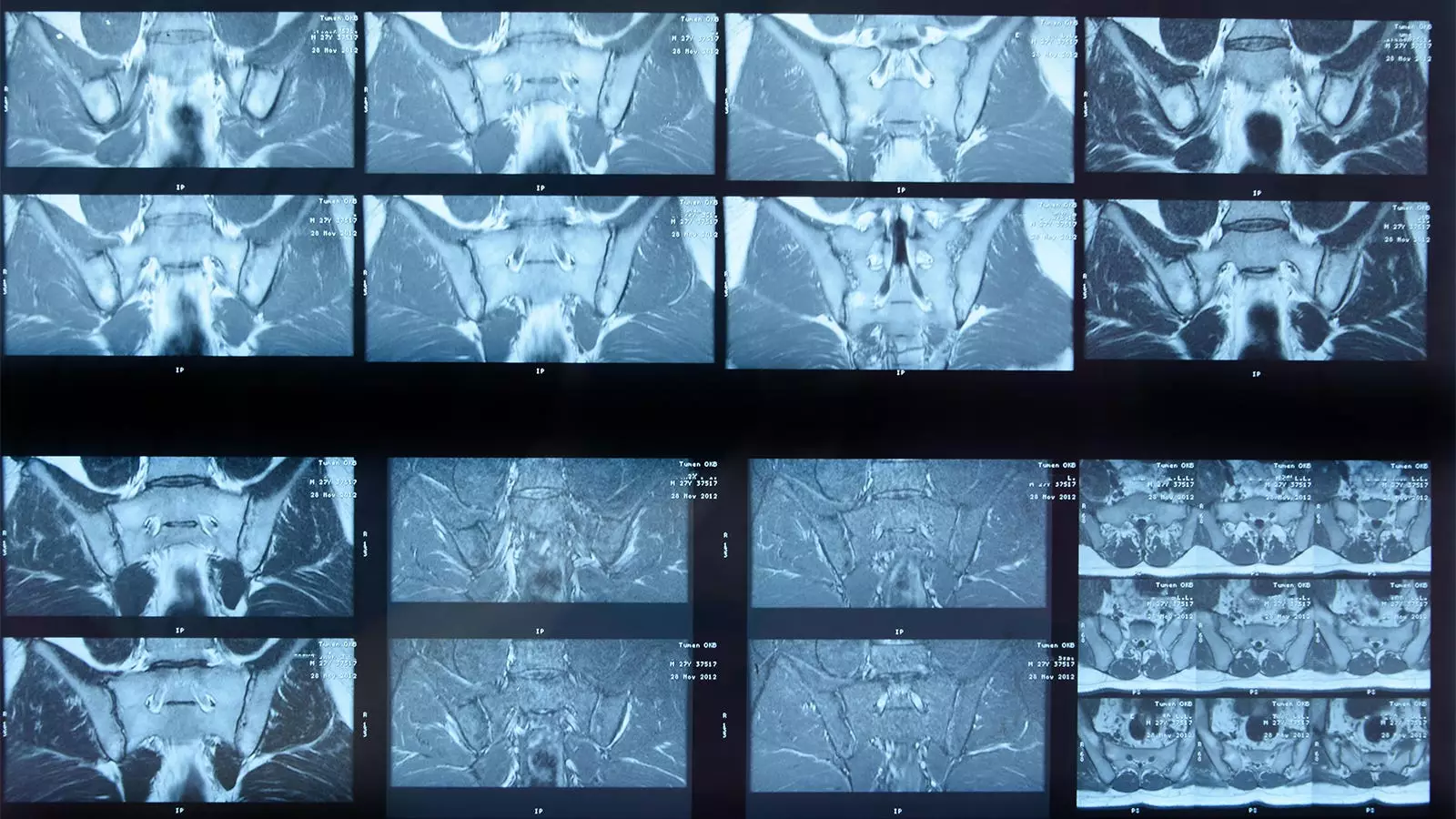
The integration of artificial intelligence (AI) into healthcare has revolutionized numerous diagnostic processes, especially in imaging analysis. One such innovation is a deep learning algorithm designed to analyze MRI scans for indications of sacroiliac joint (SIJ) inflammation in patients diagnosed with axial spondyloarthritis (axSpA). Despite promising capabilities, this AI system’s performance has exposed several areas for improvement, reflecting ongoing challenges in marrying technology with clinical expertise.
In a recent study led by Joeri Nicolaes, PhD, of UCB Pharma in Brussels, researchers put the AI algorithm to the test against expert human readers—three seasoned panelists served as the gold standard in interpreting 731 MRI images from late-stage axSpA patients. Out of these, the AI matched with human experts on detecting inflamed SIJs in 543 images. This included 304 cases of confirmed inflammation and 239 where no inflammation was observed. However, the algorithm faced significant challenges, missing inflammation in 132 cases while incorrectly flagging it in an additional 56.
Statistically, the AI demonstrated an absolute agreement of 74%, with a sensitivity of 70% and specificity of 81%. Although these figures suggest a basic level of reliability, they also raise alarms regarding the AI’s diagnostic limitations in clinical settings. Highlighting an important caveat, the research team discussed that the criteria for defining inflammation were quite conservative. This aspect alone invites scrutiny into whether the algorithm can capture the nuances of real-world clinical indications, where contextual clinical information is often paramount.
A critical perception of the AI’s capabilities stems from a combination of factors that suggest higher levels of expertise among the research panel as opposed to typical practitioners like general rheumatologists and radiologists. The algorithm’s reliance on binary categorizations might not accommodate the variability inherent in clinical practice, where human readers often utilize additional data—such as serum levels of C-reactive protein (CRP) or HLA-B27 presence—in their assessments. Therefore, while the AI might produce more standardized interpretations, it is essential to recognize that real-world applications may involve additional contextual elements that the AI currently overlooks.
Moreover, notable limitations persist regarding the algorithm’s ability to interpret structural damage visible in MRI scans, a crucial component that clinicians factor into treatment decisions for axSpA. This gap indicates that the algorithm, although useful, cannot entirely replace the nuanced understanding that experienced medical professionals bring to the table.
The AI’s performance was validated using a large unrelated cohort, derived from two extensive clinical trials: RAPID-axSpA and C-OPTIMISE. These studies enrolled individuals with active axSpA, although it is worth noting that the AI could not process scans from 137 patients due to limitations in image sizes or slice counts. Such constraints highlight potential issues in deploying AI across diverse clinical settings, which might use varying imaging protocols or equipment standards.
The challenges faced in this study underscore the necessity for continual updates to algorithms as classification criteria and imaging techniques evolve. Researchers are tasked with refining AI systems to enhance compatibility with various datasets without compromising accuracy.
While the current study presents a mixed bag of findings for the AI algorithm, it opens the door for further avenues of investigation. Future research must strive to address performance concerns, such as enhancing sensitivity and specificity levels while integrating additional data points that may assist the AI in making more informed diagnoses.
Moreover, building algorithms that can not only detect inflammation but also analyze structural changes will significantly bolster clinical utility. Such advancements could enable a more comprehensive approach to managing axSpA, facilitating timely interventions by accurately capturing systemic changes in patient conditions.
In summation, while this deep learning AI demonstrates an acceptable level of efficacy in detecting SIJ inflammation in axial spondyloarthritis, significant hurdles must be addressed before it can operate as an autonomous diagnostic tool. The insights gleaned from this study serve to bridge the gap between cutting-edge technology and the indispensable role of human expertise in medicine. As AI research progresses, it remains critical to establish a harmonious relationship between algorithms and clinicians, ensuring the best possible outcomes for patients within an increasingly digital healthcare landscape.

Leave a Reply